Microsurgical Vasectomy Reversal
Robert U. Finnerty M.D. FACS
Apart from the chances for success with reversal surgery, the single most important factor determining your chances for achieving pregnancy is the women’s age. With increasing age, fertility drops significantly, and the rate of miscarriage also rises:
[supsystic-tables id=5]
The above picture of age-related fertility decline is reflected in several studies of assisted reproductive technology. One study of healthy, fertile women undergoing artificial insemination with donor sperm indicates that the chance of getting pregnant in 12 cycles (or about a year) was 73% for women 30 and under, and dropped to 54% for women over 35.
National statistics for women undergoing in vitro fertilization using their own eggs demonstrate that the drop in IVF success is also dramatic: for women under 35, the percentage of successful IVF cycles was 41.5%; for women 35–37, it was 31.9%; for women 38–40, 22.1%; 12.4% for women 41–42; 5% for women 43–44; and just 1% for women over 44. That means that, after age 35, IVF birth rates declined about 10% every 2 years.
Note that some studies of assisted fertilization pregnancy rates suggest much higher pregnancy rates in older women. These studies typically use donor eggs from women in their 20’s, which introduces other issues, both personal and ethical.
The exact costs of assisted fertilization procedures is difficult to state exactly due to the variability from one infertility clinic to the next. The following price table is a summary of ranges obtained from a review of these prices on the web:
[supsystic-tables id=4]
I am surprised at how often this is recommended by primary care physicians; it is most definitely not a good idea!
Administering testosterone (shots, gels, patches, pills, etc.) will increase the blood levels of testosterone, but strongly inhibit the regulatory hormones FSH and LH, which results in a shutdown of sperm production. The administration of testosterone to men is in fact a very effective form of birth control! (although not ideal for many other reasons)
In many men, this condition can be treated with non-testosterone medications which stimulate the production of leutinizing hormone (LH) (which drives the production of testosterone by the testis) and follicle stimulating hormone (FSH) (which stimulates sperm production or spermatogenesis). The most common medication currently used for this is clomiphene citrate, which blocks the effects of estrogen on its receptors, resulting in an increase in both FSH and LH. This will often result in a significant improvement in testosterone, and is often associated with an improvement in sperm count.
It should be noted that this drug, although commonly used in the treatment of female infertility, is not FDA approved for treatment of low testosterone in men or male infertility, and therefore this represents an off-label use of the drug. Nevertheless it does appear to be effective in many men for this condition, and is widely used by fertility specialists, although studies suggest the improvement in pregnancy rates is modest at best.
Aromatase inhibitors such as Arimidex, which block the conversion of testosterone to estrogen, are also helpful in improving testosterone levels, but their effects on sperm production and fertility are inconsistent and often not very helpful.
It should be emphasized that the presence of low testosterone may be result of a number of clinical conditions, and a thorough evaluation by a specialist should be undertaken prior to considering these drugs.
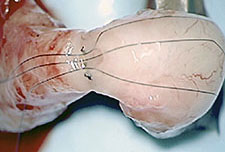
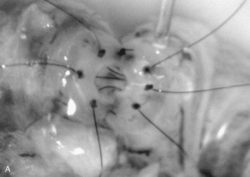 All vasectomy reversals are performed using a two-layer technique, using extremely delicate monofilament nylon microsutures (9-0 and 10-0). The “microdot” technique places small ink dots around the inner opening, and was developed to help inexperienced surgeons place the sutures evenly and accurately. Although some experienced microsurgeons use this technique, in Dr Finnerty’s experience the marking dots are unnecessary, and may in some instances result in an inappropriate number of sutures placed, depending on the individual patient anatomy.
All vasectomy reversals are performed using a two-layer technique, using extremely delicate monofilament nylon microsutures (9-0 and 10-0). The “microdot” technique places small ink dots around the inner opening, and was developed to help inexperienced surgeons place the sutures evenly and accurately. Although some experienced microsurgeons use this technique, in Dr Finnerty’s experience the marking dots are unnecessary, and may in some instances result in an inappropriate number of sutures placed, depending on the individual patient anatomy.
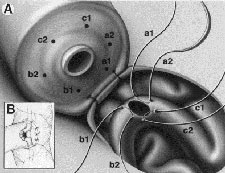 Epididymal repair is also performed in two layers, using a modification of the “intussusception technique” on the epididymal tubule. This technique was developed by Dr. Finnerty to improve the precision and success rate of this difficult and delicate repair.
Epididymal repair is also performed in two layers, using a modification of the “intussusception technique” on the epididymal tubule. This technique was developed by Dr. Finnerty to improve the precision and success rate of this difficult and delicate repair.
Conscious sedation is a technique where a local anesthetic is used to numb the surgical area, while drugs are given intravenously to make you relaxed and sleepy. Dr. Finnerty has extensive experience with this approach, but no longer uses it. The sedation can have unusual and unpleasant effects on a small percentage of patients, leading to restlessness, anxiety, and even breathing difficulty. When these side effects occur, the success of the surgery and your personal safety may be put at risk.
All reversal surgeries are now done under general anesthesia, administered by a board-certified anesthesiologist. This approach is extremely safe and comfortable, and affords the ideal environment for the successful performance of your reversal surgery.
 Dr. Finnerty uses state-of-the-art operating microscopes by Zeiss – the foremost manufacturer of these precision instruments in the world. These scopes have optical magnification up to 40x power, superb optical characteristics, and precision power focus and zoom capabilities.
Dr. Finnerty uses state-of-the-art operating microscopes by Zeiss – the foremost manufacturer of these precision instruments in the world. These scopes have optical magnification up to 40x power, superb optical characteristics, and precision power focus and zoom capabilities.
 The number of sutures used depends on the situation and the anatomy found at surgery. This question first arose when some surgeons using low-power optical loops began claiming they were doing “microsurgery.” The use of only a few larger sutures was the tip-off, as microsurgery uses finer and more numerous sutures.
The number of sutures used depends on the situation and the anatomy found at surgery. This question first arose when some surgeons using low-power optical loops began claiming they were doing “microsurgery.” The use of only a few larger sutures was the tip-off, as microsurgery uses finer and more numerous sutures.
Most experienced surgeons currently performing microsurgical vasectomy reversal use a two-layer repair on the vas, suturing the inner mucosal layer separately from the outer muscular layer. But beware of “one size fits all” answers to the “number of sutures” question — it may suggest a surgeon with less experience.
The variability in the diameter of the vas, especially the inner lumen on the testicular side, is quite large from one patient to the next. The distal lumen (above the vasectomy) is almost always between 0.2 and 0.3 mm in diameter, while the proximal lumen (below the vasectomy, closer to the testes) may vary from 0.5 mm to 1.8 mm. To precisely align the inner channel the number of inner sutures needed will vary substantially, generally between 5 and 8 sutures. In Dr. Finnerty’s experience, using more sutures than this actually increases the risk of failure, as the delicate mucosa is shredded and frayed by too many stitches, promoting scarring.
Of course, the epididymal repair is technically quite different than a vas-to-vas repair, and generally requires fewer sutures on the mucosal layer than does the vas.
Some surgeons recommend the use of anti-inflammatory medications such as naprosyn, ibuprofen, or even Prednisone (a steroid) after surgery to reduce the risk of scar tissue formation.
Dr. Finnerty does not recommend the use of these medications, as there is no medical evidence that they reduce scarring or improve surgical success rates after vasectomy reversal. While anti-inflammatory medications are generally safe and benign (in the short term), and may be useful for controlling mild postoperative discomfort, they may increase the risk of bleeding and can be hard on the intestinal tract and kidneys.
The use of Prednisone is of greater concern, as it may have serious adverse side effects, impairs wound healing, and increases the risk of infection after surgery.
Vasectomy reversal is technically demanding, and even in the most experienced of hands is sometimes unsuccessful. The best antidote to surgical scarring is a precise microsurgical repair by a surgeon with extensive experience in microsurgical vasectomy reversal.
For more information on why vasectomy reversals fail, see this page.
Sperm in the testes and duct system are normally isolated from the body’s immune system. The immune system develops in early childhood, long before sperm are present, at puberty. When a vasectomy is performed, the sperm are exposed to the immune system, and the body responds as if the sperm were a foreign protein. The immune system produces substances called antibodies against the sperm.
These antibodies may be found in the blood and on the surface of the sperm in most men after vasectomy, but generally disappear after about 6 months. In some men, however, they may remain elevated for a prolonged time.
Many infertility specialists believe these persistent sperm antibodies may cause fertility problems after a vasectomy is reversed. However, not all men with elevated sperm antibodies have problems with fertility, and other men with low or absent antibody levels are unable to achieve pregnancy. Furthermore, successful reversal should reduce the levels of sperm antibodies, through precise alignment of the duct system, eliminating exposure of the sperm to the immune system. There are several types of anti-sperm antibodies (ASA), not all of which affect sperm fertility — so reports of “high ASA levels” (usually on semen analysis) do not necessarily mean ASA fertility problems.
At this time, therefore, the role of sperm antibodies remains under investigation. Routine testing of sperm antibodies prior to surgery is not recommended, since it is expensive, and does not predict the chances for pregnancy with sufficient reliability.
In Dr. Finnerty’s opinion, persistent high sperm antibody levels after vasectomy reversal can sometimes suggest persistent partial obstruction or inaccurate alignment of the vas or epididymis reconstruction, leading to ongoing sperm exposure to the immune system.
Some surgeons use a micro-laser to assist in the reconnection of the vas. Early in his reversal experience, Dr. Finnerty performed a few reversals using this technique. In the laser technique, several sutures are placed to hold the ends of the vas together. A laser is then used to “spot-weld” the vas together, sealing only the outer layer. The laser cannot be used to align the inner layer of the vas.
The problem with this approach is the poor alignment of the inner lumen of the vas. While this approach may have a slightly better success rate than non-microsurgical vas reversal, the poor alignment of the inner layer often results in scarring and failure. The heat from the laser also tends to damage the delicate blood vessels in the vas required for healing without scar formation. Furthermore, if an epididymal repair is required, the laser cannot be used since it cannot perform the extremely delicate repair need for such a reconstruction.
Virtually all experienced microsurgeons have abandoned the use of the laser for reversal surgery because of these factors.
There is a great deal of false or misleading information about the success of vasectomy reversal, due to the poor success rates typical when reversals were done without microsurgery, and many therefore doctors as well as patients remain confused about this subject. It is also common, when doctors perform vasectomy, to emphasize its permanent nature in order to avoid hasty decisions about sterilization.
Modern microsurgical techniques allow successful reversal in almost every case, offering both high technical success and good fertility. With very few exceptions, vasectomy can be successfully revered, with excellent chances for subsequent pregnancy.
Because of the extremely small size of the sperm duct, even a perfect repair using microsurgical techniques can sometimes fail to remain open. In uncomplicated reversals where sperm is present at the time of surgery, this occurs at most about 3-4% of the time (about 1 in 25 men). In complex repairs involving the epididymis on both sides (the most difficult type of repair), failure is seen in about 15-20% of men.
Non-microsurgical reversals fail far more frequently than this.
A reversal which fails to produce sperm is very disappointing. Fortunately, in most cases repeat reversal can be done with good success rates. The chances for success depend on the reason for failure of the original surgery, and the type of reversal surgery originally performed.
Reversals generally fail for two reasons: scarring at the site of reconnection (the most common cause for failure after non-microsurgical reversals), and failure to recognize or deal successfully with epididymal blockage at the time of first surgery. If the cause of failure is scarring at the reconnection site after an uncomplicated vasovasostomy, success rates for repeat reversal are nearly identical to first time surgery. If there is an epididymal blockage, or if there has been previous surgery on the epididymis, then the success rate for repeat surgery is somewhat lower, but still very good in most cases. Repeat surgery in this situation is also quite long and may be very difficult.
Dr. Finnerty has extensive experience in complicated reversal surgery, including prior failed reversals, or difficult anatomic problems, such as vasectomy performed in the groin at the time of inguinal hernia repair.
A more detailed explanation of why reversal surgery may fail may be found here.
Most definitely! The large majority of men, even after 20 or more years, can have their vasectomy successfully reversed. Although fertility tends to decrease with longer time after vasectomy, Dr. Finnerty has seen many couples achieve pregnancy in this time frame. He has even performed a reversal on a man over 30 years after vasectomy which resulted in pregnancy.
Furthermore, the improvement in technique with more complex epididymal repairs — often required when the time after vasectomy is long — is leading not only to much better technical success, but excellent pregnancy rates as well. Time after vasectomy is becoming much less of a factor for success than it was in the past.
While it is true that the incidence of epididymal obstruction increases with time after vasectomy, partial or total epididymal blockage is actually quite common, even in men only a few years after vasectomy. Failure to address this at the time of surgery will result in higher failure rates, and even those who have sperm after surgery will tend to have much lower fertility due to poor sperm motility.
This is why it is important that your reversal surgeon have extensive experience and expertise with epididymal reconstruction, even if your vasectomy was only performed a few years ago.
In most cases, no. Almost all vasectomy techniques involve removing a short piece of the vas, and sealing off the cut ends using sutures, metal clips, cautery, or a combination of these. All of the scarring from the vasectomy — regardless of technique — is removed at the time of reversal. The length of vas removed at vasectomy is rarely if ever a problem.
The so-called “no-scalpel” vasectomy — which uses cautery alone to seal the vas — does cause, in Dr. Finnerty”s opinion, a greater chance of developing secondary epididymal obstruction. But the greatly improved success of epididymal repair using new techniques makes this issue far less important than it was in the past.\r\n\r\nOn rare occasions, a vasectomy is done at the time of an inguinal hernia repair, or an abdominal surgery. While vasectomy performed in these areas can be reversed, the surgery may be much more difficult and complicated.
While several older studies suggested an increased risk of prostate cancer in men after vasectomy, more recent studies have shown no evidence for increased risk. Other potential health problems, including heart and vascular disease, arthritis, and autoimmune disorders, have also been suspected in a few studies in the past. To date there is no conclusive medical evidence, however, that vasectomy causes these or other health difficulties.
Occasionally, a man will have problems with chronic testicular pain or discomfort after a vasectomy, due to excessive pressure in the epididymis. Vasectomy reversal is the best treatment for this relatively uncommon condition, which often responds poorly to conservative treatment such as antibiotics or anti-inflammatory medication.
Reference: NIH / NICHD summary of vasectomy risks